Seminario | Development of a new human in vitro model to study neuromuscular diseases.
Lunedì 10 luglio alle ore 15:30, in occasione degli incontri organizzati dal Dottorato in Scienze Biomediche, la Professoressa Helen Miranda ( State University of Londrina In Brazil ), presenta il seminario "Development of a new human in vitro model to study neuromuscular diseases." presso l'Aula B del Complesso Vallisneri, in via Ugo Bassi 58/B, Padova.
Abstract:
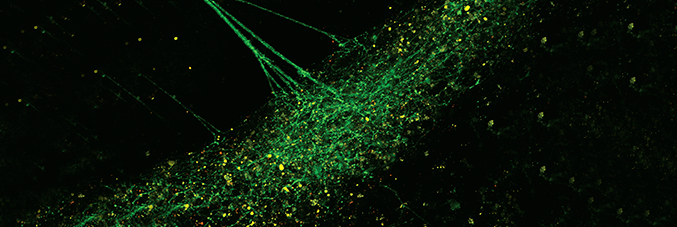
Neuromuscular junctions (NMJs) are specialized synapses that mediate the communication between motor neurons and skeletal muscles and are essential for movement. The degeneration of this system can lead to symptoms observed in neuromuscular and motor neuron diseases. Studying these synapses and their degeneration has proven challenging. Prior NMJ studies heavily relied upon the use of mouse, chick, or primary human cells; which have limited applicability for disease modeling. To enable the study of NMJ dysfunction and model specific genetic diseases, we, and others, have developed methods to generate human NMJs from induced pluripotent stem cells (iPSCs). However, published studies have highlighted limitations associated with these complexes in vitro NMJ models, including time, variability, and limited scalability. Thus, we have now developed a faster and more reproducible protocol to efficiently generate hiPSC-derived NMJs that are functional, optically responsive and scalable, enabling its use for disease modeling. In this study, we developed a robust iPSC-derived motor neurons and skeletal muscle co-culture system, which spontaneously and reproducibly form human NMJs. To our knowledge, we are the first group to apply a multiwell-multielectrode array (MEA) to quantify the activity of iPSC-derived skeletal muscles and to measure the electrophysiological activity of functional human iPSC-derived NMJs. We further leveraged our method to morphologically and functionally assess NMJs from the familial amyotrophic lateral sclerosis (ALS) iPSCs, C9orf72 hexanucleotide (G4C2)n repeat expansion (HRE), SOD1A5V, TDP43G298S and neuromuscular disease Spinal Bulbar Muscular Atrophy (SBMA). We observed a significant decrease in the numbers and activity of iPSC-derived NMJs developed from the different mutant ALS lines and in SBMA compared to their respective controls. These results demonstrate that functionally active iPSC-derived NMJs can be generated in a reproducible manner and that our approach can efficiently model specific NMJ dysfunction innate to ALS and SBMA with high sensitivity. Our newly developed method will enable the investigation of NMJs, neurodegeneration, embryonic development, homeostasis, and diseases, such as motor neuron and neuromuscular disorders. Our faster, reproducible, and scalable method is the first to be suitable for high-throughput screening.




